What do you know about Mouth Ulcers? Any pathological processes should be eliminated as early as possible. Otherwise, serious complications cannot be avoided. How to treat sores, white and red sores in the mouth on the gums of a child? This primarily depends on the severity of the symptoms, the severity of the course of the disease, and the provoking factors that contributed to the occurrence of such a condition. In addition, the age of a small patient is also important. Babies cannot point to specific complaints, so parents need to carefully monitor the behavioral changes of their son or daughter.
The implementation of simple preventive measures will help prevent pathology or significantly reduce the risk of its active progression with associated complications. Let’s look at why such symptoms appear, how inflammation is diagnosed, and how it is eliminated.

Causes of white and red sores in the mouth and on the lips of a child
Such signs indicate damage to the mucous membranes of the oral cavity and an acute inflammatory process. In this case, the etiology can be any, and the rashes can have a different appearance (color, size, shape), fullness, etc. Symptoms appear both in adults and in the smallest patients, but it is the kids who most often suffer from such an ailment.
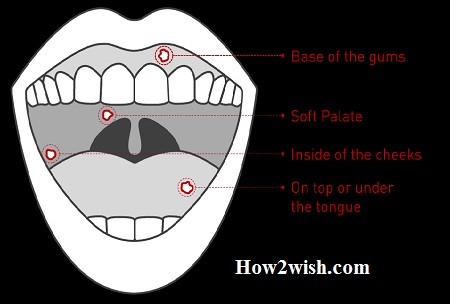
Spots appear on the inside of the cheeks, gum surfaces, tongue, and palate. They cause severe discomfort (pain, itching, burning, etc.). Preschool children have very delicate and sensitive mucous membranes. In addition, they still have insufficiently strong immunity, which is not able to fully fight viruses and protect the body from infection. For this reason, the tissues of the child react with inflammation.
Which in most cases leads to this problem:
- Poor oral hygiene;
- Pathologies of the gastrointestinal tract, which are chronic;
- Mechanical injury to the mucous membranes;
- Burns;
- Penetration of pathogenic microflora through hands, dirty toys, and other objects.
Stomatitis
Rashes occur under the influence of various factors. Most often, this leads to a decrease in the protective forces of the human body. This is caused by seasonal changes, stress, prolonged emotional stress, malfunctions in the functioning of various internal organs and systems, and chronic and acute pathologies. Often, a drop in immunity is accompanied by the development of stomatitis and herpes.
Whitish or yellowish spots up to 1 cm in size appear in the mouth (on the tongue, on the cheeks, gums, and palate). They are painful, and gradually heal, but require mandatory therapeutic intervention and special hygiene recommendations.
There are both non-contagious forms of the disease and its varieties that are easily transmitted to other people.
Injuries
As a result of mechanical or thermal action on the mucous membranes, wounds are formed, where pathogenic microorganisms penetrate. In most cases, this happens if the patient bites his nails or involuntarily pulls various objects into his mouth (for example, he likes to bite the tip of a ballpoint pen).
Anything can get hurt. At risk are people who regularly eat seeds or brush their teeth with hard brushes. Such bristles do not improve the quality of cleaning but easily injure delicate tissues. In case of damage, most often wounds and rashes in the mouth of a child or adult are formed in the area of the tongue and on the gums, where micro-traumas are localized.
The problem can also arise with malocclusion. The person will regularly accidentally bite through the inside of the cheeks and tongue. This happens with severe stress, and prolonged psycho-emotional overstrain.
Diagnostics
Only a dentist can confirm the presence of a disease. He evaluates the external manifestations, and complaints of the patient, and studies the history and results of laboratory tests. To accurately determine the type of pathogen, it is necessary to scrape biological material from the mucous membranes and send the contents for testing.
It is better not to resort to self-diagnosis at home. Only a specialist should determine the type of disease and the causes of its occurrence.
Types of stomatitis in children
There are the following types of infection in the mouth in a child or adult:
- Bacterial;
- Aphthous;
- Herpetic;
- Viral;
- Angular;
- Allergic;
- Traumatic;
- Fungal.
Children can develop any type of illness. However, babies and toddlers under the age of three most often suffer from herpes, allergies, candidiasis, and aphthous stomatitis. When the first dental units begin to erupt, there are frequent cases of a traumatic pathological process, which is caused by damage to the mucous membranes of the oral cavity.
What other criteria classify the disease:
- By location (on the lip, palate, gums, inside of the cheek, etc.);
- According to the degree of changes (deep, superficial type);
- According to the characteristics of the course (chronic, acute form).
Bacterial
It leads to the penetration of staphylococci, streptococci, and other viruses into the patient’s body. Bacteria either penetrate directly into it or enter it from chronic foci of infections, for example, from the nasopharynx, ears, lungs, and cavities affected by caries.
The Best Toothpaste to Help Fight the Effects of Pollution in Your Mouth
Aphthous
This variety in most cases appears against the background of pathologies associated with metabolic processes, the gastrointestinal tract, and due to the use of hygiene products that contain sodium lauryl sulfate.
A characteristic symptom is the rapid formation and spread of gray sores with red contours on the lips, palate, and gums in a child or adult, which cause severe pain. The disease often flows into a chronic form with constant relapses resulting from malnutrition, hormonal imbalance, and changes in blood composition.
Herpetic
This is an inflammation of the oral mucosa caused by the herpes simplex virus. Symptoms are expressed by ulcers in the mouth, migraine, and feverish manifestations. This type of stomatitis accounts for 3/4 of all infectious processes on the gums and the inside of the cheeks, palate, and tongue.
Caused by a herpes infection. Once entering the body, the virus lives there permanently. Relapses occur with respiratory diseases and a decrease in immune defense for other reasons. Rashes look like small bubbles filled with cloudy contents.

Viral
In 80% of cases, it is caused by a herpes infection discussed above. Once entering the body, the virus lives there permanently. Relapses occur with respiratory diseases and a decrease in immune defense for other reasons. Rashes look like small bubbles filled with cloudy contents.
Angular
It also bears the well-known name of the jam. Appears in patients of all ages. Reddish spots are visualized in the corners of the mouth, swelling increases, cracks are visible. The patient feels pain and burning when eating and talking.
Allergic
Adults suffer from this type of pathology in most cases after dental treatment. This is due to the reaction to anesthetics, composite materials, and prostheses. The smallest patients most often react in this way to new foods, potentially allergen foods.
Characteristic manifestations: the child has a fever and sores in the mouth with redness, burning, and itching. The rash spreads over a large area of ?? the mucous membranes.
Traumatic
The inflammatory process begins after the penetration of pathogens into the wound. It often develops during the period of eruption of milk units, as well as after poor-quality dental prosthetics or extraction.
Fungal
The most common type. It occurs due to the active reproduction in the mouth of a specific fungus of the genus Candida against the background of an imbalance of microflora, a drop in immunity, and endocrine disorders. A dense white coating appears on the soft tissues, itching is felt, and there is an unpleasant odor.
Symptoms of infection
Standard manifestations of the pathological process that patients face:
- Swelling of soft tissues;
- The formation of a white or yellowish plaque;
- Unpleasant odor from the mouth;
- Increased salivation or, conversely, excessive dryness of the mucous membranes;
- Swelling, enlargement of the lymph nodes;
- Fever.
The disease with mouth ulcers in children (from microbes or traumatic effects) is characterized by the same signs as in adults. However, some symptoms occur only in certain types of pathology. The sizes of rashes, localization, sensations of the patient, and temperature indicators differ.
In babies, fungal stomatitis, or thrush, is most common. Almost every parent observed a whitish cheesy plaque in the baby’s mouth.
Possible Complications
If you do not consult a doctor promptly, this threatens the patient with serious consequences, namely:
- Infection of ulcers, surrounding tissues, and subsequently – the whole body;
- The development of a syndrome of malabsorption, digestion of food, and hence problems with the gastrointestinal tract;
- Psycho-emotional instability;
- Fungal tonsillitis, bleeding, and inflammation of the periodontium.
How to treat children’s mouth ulcers in a child
In no case should you self-medicate? Only the attending physician should make a diagnosis and give recommendations about therapy. Attempts to cope with the disease on their own often lead to a deterioration in the well-being of babies.
To develop therapeutic tactics, it is important to conduct a thorough diagnosis and identify the causes and pathogen. The methods used should affect the disease in a complex to eliminate provoking factors and external manifestations.

Medicines of Mouth Ulcers
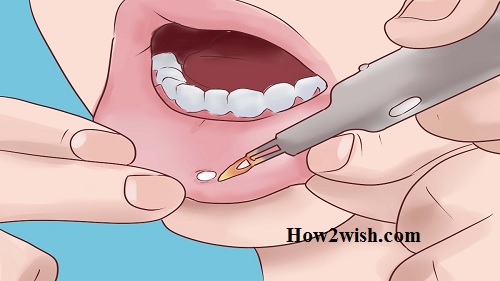
After diagnosing the inflammatory process, the dentist prescribes medications. They are symptomatic (to eliminate pain, itching, and other signs) and specialized (to combat the sources of the disease).
The first category includes:
- Vitamin and mineral complexes to increase the body’s resistance;
- Antiviral agents;
- Antipyretic;
- Anti-inflammatory drugs;
- Anesthetics;
- External compositions for the treatment of pathological foci.
Fungal inflammation is treated with special medicines based on active substances that destroy Candida pathogens. Ointments are prescribed that are safe for babies when swallowed. If an allergy is detected, antihistamines are indicated in tablet form or the form of drops, and solutions.
All mucous membranes in the mouth are subject to treatment, and not just rashes. Microorganisms are present in all tissues, and if the compositions are applied poorly, they will continue to multiply, and the therapy will take a very long time.
Ointments and gels
Children’s outdoor products should not contain an alcohol base. The best option: are Furacilin, Miramistin, and Oracept. To eliminate pain, solutions based on lidocaine are used. Hormonal creams are sometimes indicated to reduce inflammation.
For herpes, Zovirax, Acyclovir, and other ointments are prescribed. When a secondary infection is attached, antibiotics are used (for children there are not only tablets but also suspensions). From candidiasis, Candied, Fluconazole, Clotrimazole, etc. are used.
It is important not only to smear medicinal formulations but also to adhere to other rules. It is necessary to temporarily exclude solid foods from the menu, which can increase unpleasant symptoms, and also give the baby more to drink.
Rinsers and antiseptics
Both drugs sold in pharmacies and phytotherapeutic solutions and decoctions can be highly effective. They need to rinse their mouth. You can also gently lubricate the mucous membranes with a gauze swab dipped in liquid.
Folk remedies
If a child has wounds in his mouth (or “walking”, as children say), it is permissible to use home formulations, but in no case should drug therapy be abandoned. Self-prepared decoctions and infusions can be used in patients older than 2 years of age. Consider the most popular recipes.
soda and salt
You need to take ½ tsp. each substance and diluted in a glass of warm boiled water. Rinses are performed several times a day after each meal. This composition perfectly disinfects and has an anti-inflammatory effect. With fungal stomatitis, you can prepare a gruel from the same components, and then moisten gauze in it and clean off the whitish plaque from the mucous membranes.
Honey and aloe
Many people think that sores in a child’s mouth are a reason to use only unpleasant-tasting pharmaceutical drugs that cause children’s tears and tantrums. However, treatment can be more comfortable. You can grind the leaf of the plant into a gruel and add honey mass. The mixture is applied to the inflamed areas 3 times a day.
Chamomile with honey
A tablespoon of dried flowers must be brewed in 250 ml of boiling water. When the infusion has cooled, add a few teaspoons of honey there. Rinses are performed several times a day.
You can rinse your mouth with wild rose, sage, and calendula decoctions. The main thing is to consult a doctor first because not all components are safe for young children.
Prevention of Mouth Ulcers
To reduce the risk of infection, parents should:
- Thoroughly wash toys, pacifiers, bottles, and other items. The whole mouth in ulcers and abscesses in a child usually happens precisely because he sucks or gnaws contaminated things.
- Regularly carry out wet cleaning of the house. It is also extremely important to constantly ventilate the premises.
- To help strengthen children’s immunity: temper, give vitamin and mineral complexes, and monitor sleep and activity.
- Provide quality food. The diet should be varied (except for infants who are fed breast milk or adapted mixtures) and balanced.
- Wean the baby from the bad habit of chewing on various foreign objects.
- It is planned to show the child to the pediatrician and dentist (at least 2 times a year). Do not wait for the appearance of unpleasant symptoms.
Summing up on Mouth Ulcers:
If the child has mouth ulcers, inflammation, and fever, you should immediately consult a doctor. Otherwise, negative consequences cannot be avoided. At the slightest complaint and suspicion, it is worth carefully examining the baby, including his oral cavity.
In most cases, the prognosis of treatment is favorable. The most important role is played by prevention, which is mainly reduced to the protection of soft tissues from injury and compliance with hygiene recommendations.